With the hot days of summer come summer sports and outdoor activities—and more opportunities for your child to become dehydrated. Dehydration is more than just being thirsty. It's a condition where you lose more water than you take in, making it harder for your body to perform its normal daily functions. Dehydration can be dangerous if left untreated.
Whether your kids are coming home from practice, have spent a long day of play in the sun, or are getting over a stomach bug, learn to protect your child against the dangers of dehydration and heat illness.
What Puts My Child at Risk of Dehydration?
Babies and young children are at a greater risk of dehydration than adults. A child's body surface area makes up a much greater percentage of their weight than an adult's, meaning kids have a larger area to lose sweat from.
Kids often run the risk of becoming dehydrated when they're sick, especially if their symptoms include vomiting or diarrhea. But they can also become dehydrated when they're outside in hot or humid weather if they're not drinking enough water.
If you have younger children, remember that they could be at a risk of dehydration because they may not be able to communicate to you when they're thirsty.
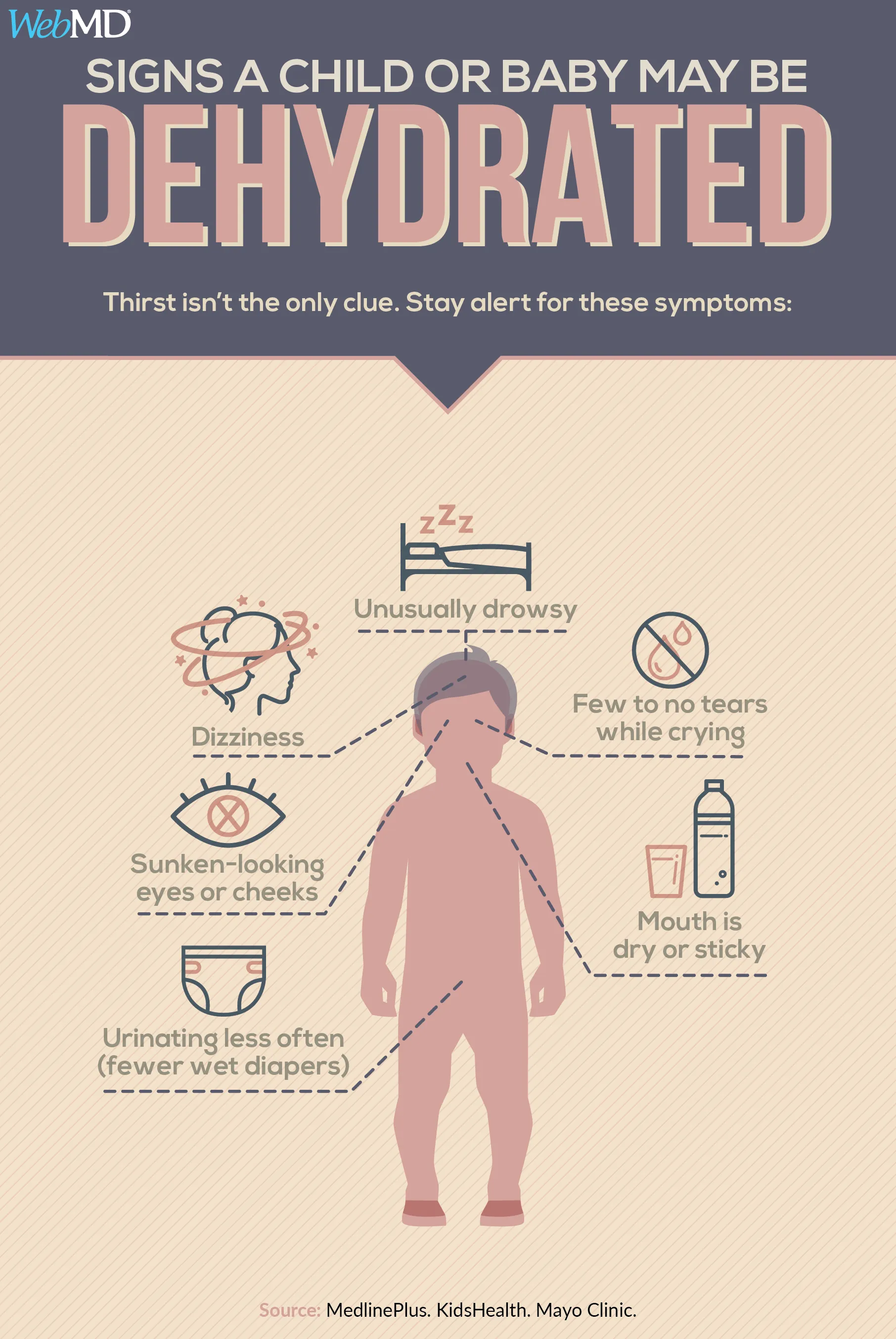
What Signs of Dehydration Should I Watch For?
Early signs of dehydration include fatigue, thirst, dry lips and tongue, lack of energy, and feeling overheated. But if kids wait to drink until they feel thirsty, they're already dehydrated. Thirst doesn't really kick in until a child has lost 2% of their body weight as sweat.
A simple rule of thumb: if your child's urine is dark in color, rather than clear or light yellow, they may be becoming dehydrated.
Untreated dehydration can lead to four worse types of heat illness:
- Heat cramps: Painful cramps of the abdominal muscles, arms, or legs.
- Heat syncope: Weakness, fatigue, or fainting after exercising in heat.
- Heat exhaustion: Dizziness, nausea, vomiting, headaches, weakness, muscle pain, and sometimes unconsciousness.
- Heat stroke: A temperature of 104 F (40 C) or higher and severe symptoms, including nausea and vomiting, seizures, disorientation or delirium, lack of sweating, shortness of breath, unconsciousness, and coma.
Both heat exhaustion and heat stroke require immediate care. Heat stroke is a medical emergency that, when untreated, can be deadly. Any child with heat stroke should be rushed to the nearest hospital.
Call your pediatrician if:
- You are worried that your child may be dehydrated.
- Your child has been vomiting for more than 12 hours or is unable to tolerate small amounts of liquids without vomiting.
- Your child has had diarrhea for more than 24 hours.
- You see signs of dehydration like dry diapers or no urine for 8 hours, dry lips, dry eyes, sunken soft spot on their head, and crying with no tears.
If you're concerned your child may have heat illness, call 911 if your child:
- Is less than 1 month old
- Is extremely sluggish
- Has skin that doesn't bounce back when pinched
- Is breathing fast
- Is confused
What Can I Do to Prevent Dehydration in My Child?
Make sure your child drinks cool water early and often. Send them out to practice or play fully hydrated. Then, during play, make sure your child takes regular breaks to drink fluid, even if they're not thirsty. The American Academy of Pediatrics recommends that an 88-pound (40-kilogram) child should drink 5 ounces of water every 20 minutes they're playing or practicing in the heat, while a 132-pound (60-kilogram) child needs to drink 9 ounces every 20 minutes. One ounce is about two kid-sized gulps.
Dehydration gets worse over time. If your child is 1% or 2% dehydrated on Monday and doesn't drink enough fluids that night, then gets 1% or 2% dehydrated again on Tuesday, that means they're 3% or 4% dehydrated by the end of the day. Dehydration will continue to build cumulatively over time.
Once the weather starts to get warmer, help your child gradually get used to being physically active in the heat. Over the course of 1 or 2 weeks, slowly increase the amount of time and the intensity of your child's outdoor activity. One small study showed that giving kids time to acclimatize to heat helped lower their risk of heat illness.
If My Child Develops Heat Illness, What Can I Do to Treat It?
The first thing you should do with any heat illness is get your child out of the sun and into a cool, comfortable place.
Have your child start drinking plenty of cool fluids, such as water or sports drinks. Sugary fruit juices or sodas with more than 8% carbohydrates are not recommended because they are not absorbed as rapidly by the body. Opt for ice chips instead. If your child vomits afterward, wait 20-30 minutes and give the fluids again. If they've vomited two or more times, call your pediatrician.
Encourage your child to take small frequent sips instead of drinking a lot at once. Offer Popsicles made with rehydration solution.
If you are concerned your infant or toddler has heat illness, do the following:
- Continue to nurse your infant if breastfeeding. Let them nurse more often and for a shorter amount of time.
- Give your baby the usual amount of fluid if bottle feeding, unless the baby is vomiting. In that case, give smaller amounts more frequently. For example, instead of 6 ounces every 4 hours, give 3 ounces every 2 hours.
- Your pediatrician may want you to give your baby small amounts of oral electrolyte solution. Check the amount with your doctor.
- Give toddlers about 1 tablespoon of oral electrolyte solution, ice chips, water, ice pops, or clear broth every 15 minutes.
After giving your child fluids, take off any excess layer of clothing or bulky equipment. You can put a cool, wet cloth on their overheated skin. In cases of heat cramps, help them gently stretch the affected muscle to relieve the pain.
Kids with heat exhaustion should be treated in the same way but should not be allowed back on the field the same day. If your child doesn't improve or can't take fluids, see a doctor.
Heat stroke is always an emergency and requires immediate medical attention.
- If your child's symptoms aren't getting better or your child continues to vomit, call your pediatrician or go to the emergency room.
- If your child is vomiting, do not give them acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Don't give aspirin to a child under 16 years.
- For mild dehydration, have your child rest for 24 hours and keep drinking fluids, even if their symptoms get better. Fluid replacement may take up to a day and a half. Continue your child's regular diet.
- For severe dehydration, your child may need IV fluids in the hospital. If you feel that your child is not improving or is getting worse, see your doctor right away.
Are Some Children More Prone to Dehydration or Heat Illness Than Others?
Some children are more at a risk of heat illness than others. One of the biggest risk factors: a previous episode of dehydration or heat illness. Other factors that can put your child at a greater risk of heat illness include obesity, recent illness (especially if your child has been vomiting or has had diarrhea), and use of antihistamines or diuretics.
Lack of acclimatization to hot weather and exercising beyond their level of fitness can also lead to heat illness in children. If your child isn't in shape, they may need more time to get used to playing in the heat.
Is It Ever Too Hot for My Child to Practice or Play Sports?
A growing number of athletic programs are creating heat acclimatization policies to ease kids into exercising in hot weather, as well as guidelines on when it's too hot to practice outside at all. Many are restricting outdoor practice when the National Weather Service's heat index rises above 104 F (40 C). The heat index, measured in degrees Fahrenheit, is an accurate measure of how hot it really feels when the relative humidity is added to the actual temperature.
If your child is spending time in the heat, make sure they're drinking plenty of water before, during, and after any activity.
